Patient’s adherence to prescribed home exercises: Barriers and interventions
Received: January 14, 2018
Accepted: March 12, 2018
Published: March 22, 2018
Genet.Mol.Res. 17(1): gmr16039898
DOI: 10.4238/gmr16039898
Abstract
Purpose: The purpose of this study is to evaluate patients’ adherence to home exercise programs in physical therapy practice in Lebanon, to learn which factors determine the level of adherence, and the methods used to promote it. Materials and methods: An online questionnaire was sent to a random group of Lebanese physical therapists. 44 respondents were included. 22 (50%) have 4-10 years of experience while the other 22 (50%) have more than 10 years of experience. The answers were submitted anonymously using an online application (Survey Monkey). Data were collected, and simple statistical analysis and calculation of percentages were performed. Results: Only 36% of respondents reported high level of adherence to home exercises among their patients. The following factors were reported to have a significant effect on adherence: age, self-efficacy, fatigue, understanding and memorizing exercises, and time. The results were in line with the data published in the literature. Among the methods used to promote adherence, verbal instructions were the most commonly used, and to a much lower extent, photos, booklets, and videos.Conclusion: Physiotherapists were highly aware of the barriers that preclude proper patient adherence to home exercises. However, their use of the available interventions is suboptimal and therefore should be emphasized.
BACKGROUND
Physical therapy plays a major role in the treatment of many disorders. Most patients receive the appropriate treatment in clinics and centers; nonetheless, this alone may not guarantee satisfactory results. The success of many treatment approaches is highly dependent on patient's compliance with home exercise programs (Bassett SF, Kolt GS and McEvoy JF, 2003, Lyngcoln A et al. 2005, Sarafino PS, 2005). More than 96% of physical therapists in the U.S. provide exercise advice or instructions to their patients (Jamison J and Rupert R, 2001, Christenson MG et al. 1993), yet only 24 to 40% of patients fully adhere to them (Sluijs EM et al. 1993, Taylor AH et al. 1996).
Adherence is defined by the World Health Organization (WHO) as: "the extent to which a person's behavior… corresponds with agreed recommendations from a healthcare provider” (WHO, 2003). Since the goal of physical therapy is to optimize patient's health, various studies were conducted to identify factors that affect patients' adherence to home exercises. Exercise performance is not directly controlled by the physical therapist, therefore predicting patient's adherence to exercises is very difficult (Bassett SF, 2003, Kolt GS and McEvoy JF, 2003, Lyngcoln A et al. 2005, Sarafino PS, 2005). Prolonged exercises and self-management are highly recommended for patients with a variety of conditions preparing them to return to their work more quickly (Airaksinen O et al. 2004).
A lot of strategies were suggested based on the probable motivators and barriers that affect patient's adherence. Self-efficacy, time, outcome expectations, patient-therapist interaction, positive and negative reinforcement, emotional distress, and characteristics of the home exercise programs (HEP) are all considered potential motivators or barriers (Chan D and Can F, 2010). Furthermore, exercise misunderstanding and forgetting are major factors that preclude patient's adherence. Therefore, there is a clear need to develop methods that facilitate patients' involvement and adherence to an independent exercise program. Those strategies must target all patients with different individual characteristics (e.g. age, sex, intelligence, etc...).
Physical therapists play a fundamental role in promoting adherence. Educating the patients about their medical condition and the consequences of sub-optimal exercises is considered an effective way for patient motivation. Patient reassessment, booklets, videos, and good patient-physical therapist relationship are all motivators for home exercising.
This study aims at assessing the adherence rate to home exercises among patients, examining factors that affect it, and assessing the interventions the physical therapists implement in order to promote adherence.
HYPOTHESIS
Based on the literature review on patient’s adherence, we noticed that most physical therapists pointed out the same type of barriers and used similar interventional methods. In fact, patient adherence to prescribed home exercises is a major requirement for cure and prolonged treatment effect. Although most patients know the importance of compliance, few of them actually do adhere.
In this study, we hypothesize that physical therapists in Lebanon know the barriers that patients face regarding HEP, and that they use appropriate interventions to motivate and facilitate this adherence.
Introduction
Physical therapy plays a major role in the treatment of many disorders. Most patients receive the appropriate treatment in clinics and centers; nonetheless, this alone may not guarantee satisfactory results. The success of many treatment approaches is highly dependent on patient's compliance with home exercise programs (Bassett SF, 2003, Kolt GS and McEvoy JF, 2003, Lyngcoln A et al. 2005, Sarafino PS, 2005). More than 96% of physical therapists in the U.S. provide exercise advice or instructions to their patients (Jamison J and Rupert R, 2001, Christenson MG et al. 1993), yet only 24 to 40% of patients fully adhere to them (Sluijs EM et al. 1993, Taylor AH et al. 1996).
Adherence is defined by the World Health Organization (WHO) as: "the extent to which a person's behavior… corresponds with agreed recommendations from a healthcare provider” (WHO, 2003). Since the goal of physical therapy is to optimize patient's health, various studies were conducted to identify factors that affect patients' adherence to home exercises. Exercise performance is not directly controlled by the physical therapist, therefore predicting patient's adherence to exercises is very difficult (Bassett SF, 2003, Kolt GS and McEvoy JF, 2003, Lyngcoln A et al. 2005, Sarafino PS, 2005). Prolonged exercises and self-management are highly recommended for patients with a variety of conditions preparing them to return to their work more quickly (Airaksinen O et al. 2004).
A lot of strategies were suggested based on the probable motivators and barriers that affect patient's adherence. Self-efficacy, time, outcome expectations, patient-therapist interaction, positive and negative reinforcement, emotional distress and characteristics of the home exercise programs (HEP) are all considered potential motivators or barriers (Chan D and Can F, 2010). Furthermore, exercise misunderstanding and forgetting are major factors that preclude patient's adherence. Therefore, there is a clear need to develop methods that facilitate patients' involvement and adherence to an independent exercise program. Those strategies must target all patients with different individual characteristics (e.g. age, sex, intelligence, etc...).
Physical therapists play a fundamental role in promoting adherence. Educating the patients about their medical condition and the consequences of sub-optimal exercises is considered an effective way for patient motivation. Patient reassessment, booklets, videos and good patient-physical therapist relationship are all motivators for home exercising. This study aims at assessing the adherence rate to home exercises among patients, examining factors that affect it, and assessing the interventions the physical therapists implement to promote adherence.
Methods
Participants
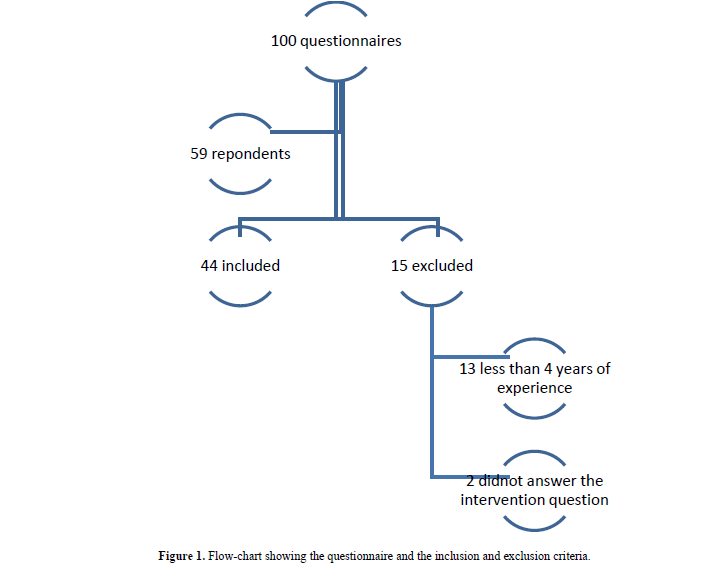
After developing a questionnaire adapted from Slujis (1993) (Sluijs EM et al. 1993) (Figure 1), we used the Survey Monkey online application and send the link through WhatsApp mobile application to 100 random physical therapists after calling each of them and obtaining a verbal consent. 59 subjects completed the questionnaire. They were then screened with inclusion and exclusion criteria. 44 were included and 15 were excluded. In this study the participants were categorized according to their years of experience into 2 groups (less than 10 years and more than 10 years) to compare their way of intervention in correlation to their experience.
Inclusion criteria
The included participants follow these criteria:
• Physical therapists
• 4 and more years of experience
• Answered the intervention question
Exclusion criteria
• Less than 4 years of experience
• Did not answer the intervention question
Among the respondents, 15 were excluded. 13 were excluded because they have less than 4 years of experience; 2 were excluded because they did not answer the intervention question.
Statistical Analysis
Statistical methods were applied to calculate percentages. Pie charts were used to display the results as well as comparative Table 1 below.
| Feeling tired | 65% | 35% |
| Inability to perform them | 43% | 57% |
| Forgetting to do them | 81% | 19% |
| Forgetting how to do them | 64% | 36% |
| Not having enough time | 75% | 25% |
| Exercises not fitting their daily routine | 48% | 52% |
| Not believing that exercises are helpful | 14% | 86% |
Table 1. The barriers that the patients face regarding HEP.
Results
Which barriers do patients report to face regarding home exercises?
65% of PT answered that their patients do not adhere because feeling tired.
81% answered because their patients forget to the exercises while 64% because the forget how to do the exercises.
75% of the physical therapists mentioned that not having enough time is a barrier for not adhering.
86% of the PT stated that their patient believe that exercises are helpful for increasing their health status.
Sub-group study
Among the 44 participants, 22 have 4-10 years of experience and 22 have more than 10 years. When comparing both groups we notice that: 36% of PTs who had less than 10 years of experience mentioned that they use only verbal instructions while 56% for those who had more than 10 years of experience. 41% of PTs who had less than 10 years of experience uses verbal instructions with other methods while 36% for more than 10 years. Both groups use videos at the same percentage (14%) (Table 2).
| Intervention | Less than 10 years | More than 10 years |
|---|---|---|
| Pure verbal | 36% | 56% |
| Verbal with other intervention | 41% | 36% |
| Photos | 41% | 36% |
| Videos | 14% | 14% |
| Booklet | 27% | 9% |
Table 2. Showing the results when comparing the methods of intervention between the 2 groups (more than 10 years and less than 10 years respectively)
Discussion
Physical therapy plays an important role in the treatment of many disorders. Although many patients receive the appropriate treatment, not all get optimal results. The success of many treatment approaches is highly dependent on patient compliance to home exercises. As noted previously, various studies have been conducted to identify the barriers that preventing patient from adherence and suggest the appropriate strategies that overcome these barriers.
Barriers
Tiredness and time: The participants answered that 65% and 75% of patients report feeling tired and lack of time respectively as being barriers. Lazo et al. (2003) stated that among patients who are not committing to exercises, 80% cited that lack of time is the reason (Lazo MG et al. 2003), which is comparable with the results of our study. Many other studies also confirm this result, where Ogwumike et al. (2014), Francesc et al. (2009) and Were Basset et al. (2003) all mentioned that decreased time and patient tiredness were among the major barriers that the patient faces regarding home exercise adherence (Ogwumike O et al. 2014, Francesc M et al. 2009, Bassett SF, 2003, Mayo NE, 1978)
This highlights how important is that physical therapists take into consideration the life style of patients when recommending exercises. They should tailor an exercise plan to every patient based on his occupation, abilities, and economic status.
Self-efficacy: There is a significant relation between self-efficacy and adherence to home exercises. Studies showed that patients who have high self-efficacy tend to adhere more to HEP. In his study, Rensik et al. (2001) found that the elderly tends to have more adherences when they believe that they can walk safely and recognize well the exercise benefit (self-efficacy) (Rensik B et al. 2001).
In our study, 80% of physical therapists stated that patients report to them the problem they face regarding home exercises and 86% stated that their patients think that exercises are useful. This indicates that the patients that therapists deal with have high self-efficacy. Being aware of any complaints the patient reports regarding HEP is the key that PT can use in motivating and boosting the internal locus (discussed previously) and as a result the self-efficacy of the patient.
Allowing patients to do exercises by their own gives them a sense of self control which increases his self-efficacy. This does not mean that they should not be constantly provided with encouragement and support.
Forgetting exercises: 81% of physical therapists stated that their patients forget to do their exercises while 64% forget how to do them. This result was emphasized by both Kellie et al. (2015) and Turk (1991) who noticed that exercise memorizing is important for exercise adherence (Kellie R et al. 2015, Turk DC and Rudy TE, 1991). Chan D (2010) stated that 60% of all therapists do frequent reassessment of patient exercise performance (Chan D and Can F, 2010); this is like what we found in our study (57%). During every session the physical therapist has to ask the patient to perform the learned exercise in front of him as a reminder and to point out any errors. Other means to target this problem are discussed later.
Exercise severity: As mentioned previously, 65% of physical therapists in our study reported that their patients complain of feeling tired while 75% mentioned that their patients had no time to afford exercises. These two factors are highly interconnected with the number and severity of exercises. Medina et al. (2009) discerns that the HEP characteristics, especially the number of exercises given, contribute to the adherence of HEP (Medina F et al. 2009). Henry et al. (1999) found that when fewer exercises are given, elderly would become more adherent to HEP (Henry KD et al. 1999). Multiple studies state that the optimal number of exercises given should be 2 or 3 exercises (Kellie R, 2015, Ley P, 1979). When prescribing HEP the PT should take the severity of exercises in to consideration. When given fewer and easier exercises, shorter time and less effort are needed, which leads to better adherence and more effective treatment
Age: In our study, physical therapists cited that 9% of patients aging between 15-25 years do adhere. The same figure is reflected for patients older than 45 years, since 18% of them were reported to comply. Interestingly 73% stated that mid-aged patients (26 – 44 yrs) adhere the most. In young patients that may be due to the more distracted life and the decreased awareness of their health status. In contrast, in the elderly age group this may be contributed to decreased health capabilities, decreased memory, and limited ability to perform exercises correctly. When prescribing HEP to patient, his age should be considered. For more elderly patients simple and easy exercises should be given, while for younger patients the PT should select more enjoyable exercises.
Interventions: In our study 84% of physical therapists admitted that they prescribe HEP in a regular manner, while only 36% of patients commit highly to them (Graph 5). This indicates that the PT should create and modify their strategies to improve patient compliance.
Verbal instructions: A major responsibility of physical therapy is to motivate, promote, prescribe, explain, and educate about home exercises and their importance as this is highly related to the promotion of patient health. Providing sufficient explanation about the diagnosis and prognosis of the patient disease will put him in the atmosphere of the treatment plan, which will affect positively his compliance. When providing this explanation, it is important to focus on the importance of physical therapy during treatment. This will optimize the patient’s expectations from physical therapy and will help him be part of the treatment plan. Part of this education consists of the verbal instructions that are provided. Physical therapists are required to provide information about indications, contraindications, and specifications of home exercises to patients each according to his case. We found that 82% of physical therapists provide verbal education to patients. Among these, 45% use verbal instructions exclusively. Patients who receive exclusively verbal instructions may face misunderstanding, forgetting to do or how to perform the exercise, and lack of motivation. This result was confirmed by a study made by Mc Lean et al. which states that verbal instructions improve short term compliance (less than 2 weeks) (Mc Lean et a, 2010). Verbal instructions have a major role in educating the patient and improving his self-efficacy. They help as well in strengthening the therapist-patient interaction. Nonetheless, they should not be used alone. Exclusive verbal instruction may lead to misunderstanding of the exercise, forgetting and may decrease the patient interest in performing the exercise.
Booklets: In our study, only 18% of physical therapists reported that they use booklets. This percentage is significantly low considering the proven effectiveness of booklets in fostering patients’ adherence. Schneiders et al. (1998) stated that patients who received additional written and illustrated instructions had a significantly higher mean compliance (77.4%) compared to the group that received verbal instructions alone (38.1%) (Schneiders AG et al. 1998).
Given the wide variety of conditions, preparing booklets for each of them is not feasible. Therefore, it is reasonable to prepare standard booklets for the most commonly treated cases (fractures, ACL injuries, etc.) and to have them available to all physical therapists in their clinics.
Videos: Videos might be more helpful during early sessions to educate the patient about their cases, increase his involvement, and eliminate any misunderstanding of home exercises. Pavlou et al. (2013) found that videos alone are not sufficient in improving HEP adherence (Pavlou M et al. 2013). This result was supported by Lysack et al. (2005) and Basler et al. (2007) who found that videos are not superior to other strategies (Lysack et al. 2005, Basler HD et al. (2007). In our survey only 11% of physical therapists used videos as part of education. This may be related to the lack of such resources or difficulty accessing them and highlights the importance of developing standardized videos available for use by physical therapists.
Photos: In our survey a fair percentage (41%) of physical therapists mentioned that they use photos as an intervention. Schneider et al. stated that when combining photos and writing 76% of the patients had adhered (Medina-Mirapex F, 2009). Therefore, using illustrations should be essential for physical therapists who seek optimal adherence for their patients. Clarification photos with clear verbal or written instructions could be sufficient for the patient to understand the exercise.
Patient condition: In our study we noticed that the physical therapists prescribe exercises for musculoskeletal disorders (95%) much more commonly than other medical cases such as cardiopulmonary (16%) and neurological (36%) regardless of the fact conditions other than musculoskeletal are as important. Every medical care needs to be treated independently and requires patient involvement in physical therapy sessions. Physical therapists should be more aware of these cases and give them sufficient care. This starts with increasing the awareness of the importance of targeting conditions other than musculoskeletal disorders.
Years of experience: There seems not to be a major difference between more experienced and less experienced physical therapists when it comes to the type of methods applied (Table 2). This highlights the need to target both groups in the attempt to implement newer strategies, to update the educational system, and to focus on workshops that promote awareness of the variety of interventions that should be used.
Conclusion
This study clearly highlights the type of practice of a random sample of physiotherapists in Lebanon. It also gives an idea about their perception of the barriers their patients face and limit their adherence to home exercises. The busy life with limited time is the first barrier. It is suggested that the physical therapist limits the number of exercises to 2-3 exercises and always adds new exercises and delete old ones. Many studies showed that mid-age is the best age for patient adherence, hence the physical therapist should have a special emphasis on the younger and older patients. Frequent reassessments and reviewing of exercises are essential in helping the patient memorize the exercises and perform them in an appropriate manner.
Finally, our study obviously shows that the array of interventions physical therapists are implementing is sub-optimal. Verbal instructions with good education are the most commonly used. However, a greater emphasis should be put on other methods such as booklets and written instructions, photos, and videos. Based on a case-by-case approach, a combination of those strategies is recommended to ensure the best outcomes.
The main limitations of our study are the possibility of recall bias among the participants and the relatively low sample size. This study, on the other hand, is a pioneering study that addresses the perception and practice of Lebanese physical therapists concerning patient adherence to home exercises. Additionally, the sample is random and includes participants with different experience, educational backgrounds and levels, and location of practice. Finally, it does not limit its scope to describing the problem but also reviews and suggests solutions based on the literature.
RECOMMENDATIONS
It is recommended to conduct a similar study by using another questionnaire that targets patients. This will complete the picture and help us understand the barriers from the patient’s point of view and their perception of the effectiveness of various interventions that promote adherence.
About the Authors
Corresponding Author
Khodor Haidar Hassan
Department of Physical Therapy, Faculty of Public Health, Lebanese University, Hadath, Lebanon
- Email:
- drkhodorhaidar@hotmail.com
References
- Airaksinen O (2004) European guidelines for the management of chronic nonspecific low back pain. European spine journal. 15: 192-300.
- Basler HD (2007). TTM based counselling in physiotherapy does not contribute to an increase of adherence to activity recommendations in older adults with pain a randomized controlled trial. European Journal of Pain. 11(1): 31. https: //doi.org/10.1016/j.ejpain.2005.12.009
- Bassett SF (2003). The assessment of patient adherence to physiotherapy rehabilitation. New Zeal J Physiother. 31: 60-66.
- Bramley TJ, Gerbino PP, Nightingale BS, Frech-Tamas F (2006). Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organizations. J Manag Care Pharm. 12: 239-245. https: //doi.org/10.18553/jmcp.2006.12.3.239
- Brekke HK, Sunesson A, Axelsen M (2004). Attitudes and barriers to dietary advice aimed at reducing risk of type 2 diabetes in first-degree relatives of patients with type 2 diabetes. J Hum Nutr Diet. 17: 513-521. https: //doi.org/10.1111/j.1365-277x.2004.00566.x
- Burton LC, Shapiro SB, German PS (1999). Determinants of physical activity initiation and maintenance among community-dwelling older persns. Prev Med. 29: 422-430. https: //doi.org/10.1006/pmed.1999.0561
- Chan D and Can F (2010). Patients’ adherence/compliance to physical therapy home exercises. Fizyoter Rehabil.21(3): 132-139.
- Chatzisarantis NLD, Hagger MS, Smith B (2007). Influences of perceived autonomy support on physical activity within the theory of planned behavior. European Journal of Social Psychology. 37(5): 934-954. https: //doi.org/10.1002/ejsp.407
- Cline CM, Bjorck-Linne AK, Israelsson BY (1999). Non-compliance and knowledge of prescribed medication in elderly patients with heart failure. Eur J Heart Fail. 1: 145-149. https: //doi.org/10.1016/s1388-9842(99)00014-8
- Christenson MG and Morgan DRD (1993). Job analysis of chiropractic in Canada: A report, survey, analysis, and summary of the practice of Chiropractic within Canada. Greely, CO: National Board of chiropractic examiners.
- Engström LO (2005). Patient adherence in an individualized rehabilitation programme: A clinical follow-up. Scandinavian Journal of Public Health. 33(1): 11-18. https: //doi.org/10.1080/14034940410028299
- Francesc M (2009). Personal Characteristics Influencing Patients’ Adherence to Home Exercises Deuring Chronic Pain: A Qualitative Study. J Rehabil Med. 41: 347-352. https: //doi.org/10.2340/16501977-0338
- Gecht MR, Connell KJ, Sinacore JM, Prohaska TR (1996). A survey of exercise beliefs and exercise habits among people with arthritis. Arthritis Care Res. 9(2): 82-88. https: //doi.org/10.1002/1529-0131(199604)9: 2<82: : aid-anr1790090203>3.0.co;2-t
- Gerard J (1999) Tortora principles of anatomy and physiology, 13th edition. 1: 628-629.
- Henry KD, Rosemond C, Eckert LB (1999). Effect of number of home exercises on compliance and performance in adults over 65 years of age. Phys Ther. 79(3): 270-277. https: //doi.org/10.1093/ptj/79.3.270
- Howard DB and Gosling CM (2008). A short questionnaire to identify patient characteristics indicating improved compliance to exercise rehabilitation programs: A pilot investigation. Int’l. J. Osteopathic Med. 11(1): 7-15. https: //doi.org/10.1016/j.ijosm.2007.12.002
- Jamison J and Rupert R (2001). Maintenance care: towards a global description. J Can Chiropr Assoc. 45(2): 100–105.
- Kolt GS and McEvoy JF (2003). Adherence to Rehabilitation in patients with low back pain. Man Ther. 2003: 8: 110-116. https: //doi.org/10.1016/s1356-689x(02)00156-x
- Karnad P and McLean S (2011). Physiotherapists’ perceptions of patient adherence to home exercises in chronic musculoskeletal rehabilitation. International Journal of Physiotherapy and Rehabilitation.
- Kellie R and Stickler (2015). Adherence to Physical Therapy: A Qualitative Study. JSPTR.1(1).
- Kravitz RL, Hays RD, Sherbourne CD (1993). Recall of recommendations and adherence to advice among patients with chronic medical conditions. Arch Intern Med, 153: 1869-1878. https: //doi.org/10.1001/archinte.153.16.1869
- Lazo MG, Filipinas SG, Valdez JR, Poster JR (2003). Compliance with home exercise programs: a preliminary report. Archives of Physical Medicine and Rehabilitation. 84(9): E29
- Leslie R (2005). The challenge of patient adherence. Therapeutics and Clinical Risk Management. 1(3) 189-199.
- Ley P (1979). The use and improvement of written communication in mental health care and promotion. Psych Health Med. 18: 245-55. https: //doi.org/10.1080/13548509808400589
- Lyngcoln A, Taylor N, Pizzari T (2005). The relationship between adherence to hand therapy and short-term outcome after distal radius fracture. J Hand Ther. 18: 2-8. https: //doi.org/10.1197/j.jht.2004.10.008
- Lysack C (2000). A compliance and satisfaction with home exercise: a comparison of computer assisted video instruction and routine rehabilitation practice. Journal of Allied Health. 34(2): 76e82
- Mayo NE (1978). Patient compliance: practical implications for physical therapists. A review of the literature. Phys Ther. 58: 1083-1090. https: //doi.org/10.1093/ptj/58.9.1083
- McLean (2010). Interventions for enhancing adherence with physiotherapy: a systematic review. Manual Therapy. 15(6): 514-521. https: //doi.org/10.1016/j.math.2010.05.012
- Medina-Mirapex F (2009). Predictive factors of adherence to frequency and duration components in home exercise programs for neck and low back pain: An observational study. BMC Musculoskeletal Disorders.10: 155-164. https: //doi.org/10.1186/1471-2474-10-155
- Moore JE, Von Korff M, Cherkin D (2000). randomized trial of a cognitive-behavioral program for enhancing back pain self-care in a primary care setting. Pain. 88: 145-153. https: //doi.org/10.1016/s0304-3959(00)00314-6
- Näslund GK, Fredrikso, M, Hellénius M, de Faire U, et al. (1996). Determinants of compliance in men enrolled in a diet and exercise intervention trial: a randomized, controlled study. Patient Education and Counseling. 29(3): 247-256. https: //doi.org/10.1016/s0738-3991(96)00917-2
- Ogwumike O (2014). International journal of therapies and rehabilitation research. 3: 1
- Pavlou M (2013). Randomized trial of supervised versus unsupervised optokinetic exercise in persons with peripheral vestibular disorders. Neurorehabil Neural Repair. 27: 208-218. https: //doi.org/10.1177/1545968312461715
- Pisters MF, Veenhof C, Schellevis FG, Twisk P, et al. (2010). Exercise adherence improves long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res. 62: 1087. https: //doi.org/10.1002/acr.20182
- Resnick B (2001). Testing a model of exercise behavior in older adults. Res Nurs Health. 24: 83-92. https: //doi.org/10.1002/nur.1011
- Rost K, Roter D, Bertakis K (1990). Physician-patient familiarity and patient recall of medication changes. The collaborative study group of the SGIM task force on the doctor and patient. Fam Med. 22: 453-457.
- Sarafino PS (2005). Health Psychology: Biopsychosocial interactions. 5th edition. New Jersey; John Wiley & Sons Inc. 236-265.
- Schoo AMM, Morris ME, Bui QM (2005). The effects of mode of exercise instruction on compliance with a home exercise program in older adults with osteoarthritis. Physiotherapy. 91(2): 79-86. https: //doi.org/10.1016/j.physio.2004.09.019
- Schneiders AG, Zusman M, Singer KP (1998). Exercise therapy compliance in acute low back pain patients. Manual Therapy.
- Shemesh E, Shneider BL, Savitzky JK (2004). Medication adherence in pediatric and adolescent liver transplant recipients. Pediatrics. 113: 825-832.
- Shilpa B, Gaikwad (2016). Home exercise program adherence strategies in vestibular rehabilitation: a systematic review, a Department of Allied Health Studies, School of Allied Health Professions, Loma Linda University, Loma Linda, CA, USA. 5 (2): 53-62
- Sluijs EM, Kok GJ, van der Zee J (1993). Correlates of exercise compliance in physical therapy. Phys Ther. 73: 771-782. https: //doi.org/10.1093/ptj/73.11.771
- Sweeney S, Taylor G, Calin A (2002). The effect of a home-based exercise intervention package on outcome in ankylosing spondylitis: a randomized controlled trial. J Rheumatol. 29: 763-766.
- Taylor AH and May S (1996). Threat, and coping appraisal as determinants of compliance with sports injury rehabilitation: An application of protection motivation theory. J Sport Sci. 14: 471-482. https: //doi.org/10.1080/026404196367606
- Turk DC and Rudy TE (1991). Neglected topics in the treatment of chronic pain patients- relapse, noncompliance, and adherence enhancement. Pain. 44: 5-28. https: //doi.org/10.1016/0304-3959(91)90142-k
- Waddell G, Newton M, Henderson I, Somerville D, et al. (1993). A fear-avoidance belief questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 52(2): 157-168. https: //doi.org/10.1016/0304-3959(93)90127-b
- Whitlock EP, Orleans CT, Pender N, Allan J, et al. (2002). Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med. 22(4): 267-284. https: //doi.org/10.1016/s0749-3797(02)00415-4
- World Health Organisation (2003). Adherence to long-term therapies evidence for action: Evidence for action. WHO library; Switzerland.
- Zaghloul SS and Goodfield MJ (2004). Objective assessment of compliance with psoriasis treatment. Arch Dermatol. 140: 408-414.
- Zunker C and King WC (2012). Psycho-social assessment and treatment of bariatric surgery patients. Psychology Press and Routledge, part of the Taylor and Francis Group; London: 2012. Physical Activity Pre and Post-Bariatric Surgery. pp: 131-158.
Keywords:
Download:
Full PDF- Share This