Abstract
Evolution of CD4+CD25hi T cell subsets in Aspergillus-infected liver transplantation recipients reduces the incidence of transplantation rejection via upregulating the production of anti-inflammatory cytokines
Author(s): T. Xing, L. Zhong, G. Qiu, L. Huang and Z. PengInfection is the leading risk factor of liver transplantation-related death. Aspergillosis is a life-threatening complication in immune-compromised patients, and is the cause of approximately 2/3 of deaths in liver transplant recipients. In our previous studies, we found a regulatory T cell (Treg) population that showed significantly increased immune tolerance in Aspergillus-infected liver transplant recipients. Furthermore, interleukin (IL)-17 production was also increased, and an IL-17-producing Treg cell subset was identified in these patients. Functional studies of the role of these IL-17-producing Treg cells in the induction of immune tolerance are needed to help reduce the death rate of liver transplantation recipients. This study included 75 liver transplant recipients with and without histologically confirmed aspergillosis after liver transplantation. The percentage of T cell population subsets producing cytokines was detected by fluorescence-activated cell sorting and enzyme-linked immunosorbent assay in peripheral blood. Complements in blood serum were also examined. The risk of acute rejection was lower in Aspergillus-infected liver transplant recipients compared to the non-Aspergillus-infected group; the CD4+CD25hi T cell population in peripheral blood was higher and the CD4+CD45RA-CD45RO+ T cell population was lower. There was no significant difference between the CD4+CD25loCD45RA+ and CD4+CD25loCD45RA- T cell populations. Moreover, IL-6 decreased and IL-4 increased in the blood serum of Aspergillus-infected liver transplant recipients. Together, these results indicate that the incidence of graft rejection in liver transplantation recipients with Aspergillus infections was lower than that of the non-infected group, and suggests a mechanism for this effect.
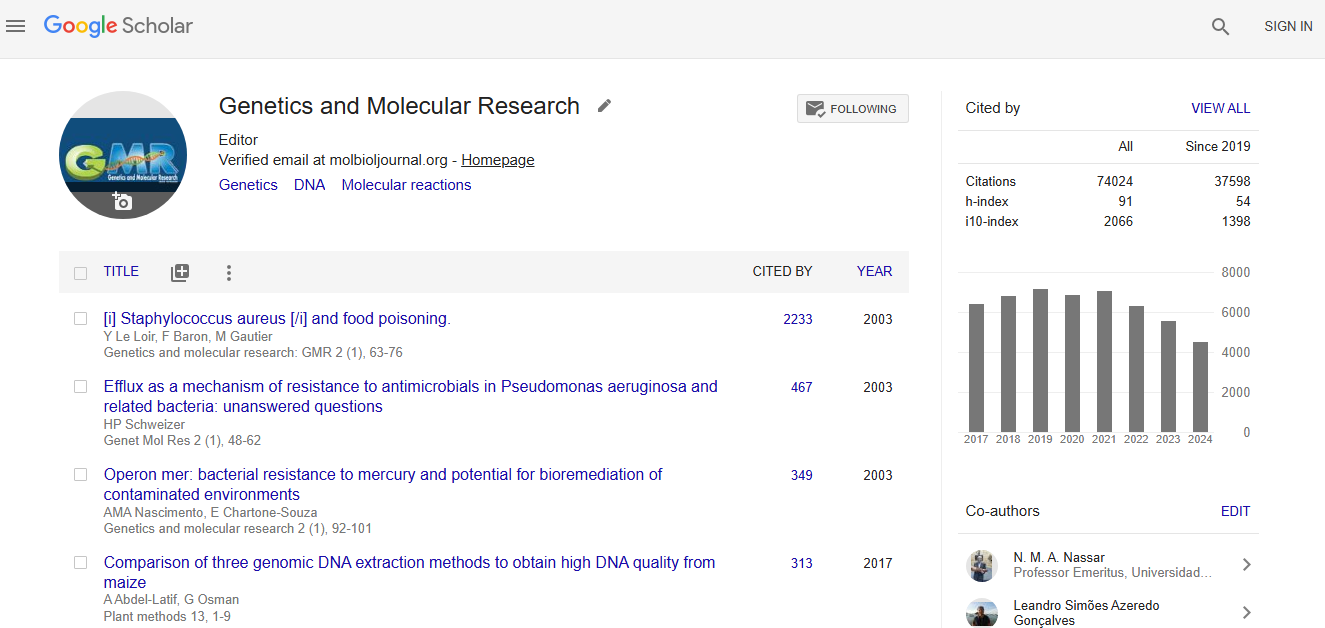
Impact Factor an Index
Google scholar citation report
Citations : 74024
Genetics and Molecular Research received 74024 citations as per google scholar report